Georgia Tech ECE Assistant Professor Shaolan Li is part of a team of engineers, data scientists, and medical clinicians led by the Cockrell School of Engineering at The University of Texas at Austin that has been awarded a grant from the National Science Foundation's ASCENT program. The purpose of this project is to develop a wearable device for patients with pneumonia, allowing medical personnel to track their progress remotely and use data to predict how their condition may change.
Pneumonia has emerged as a life-threatening complication of COVID-19, accounting for nearly half of all patients who have died from the novel coronavirus in the U.S. since the beginning of the pandemic. Even before the onset of the COVID-19 pandemic, pneumonia was responsible for more than 43,000 deaths in 2019.
Monitoring pneumonia remains a challenge because it manifests itself differently in almost every patient and can develop in any patient infected by coronavirus. The Georgia Institute of Technology is part of a team of engineers, data scientists, and medical clinicians led by the Cockrell School of Engineering at The University of Texas at Austin that has been awarded a grant from the National Science Foundation's ASCENT program. The purpose of this project is to develop a wearable device for patients with pneumonia, allowing medical personnel to track their progress remotely and use data to predict how their condition may change.
This project combines state-of-the-art technology across wearable devices, integrated circuits and machine learning. And the larger goal is to develop ways to safely monitor patients remotely and maintain high-quality care, wherever they are.
"We hope to solve this global challenge of achieving pervasive surveillance of patients, whether they're in the hospital, out in the world or quarantining at home in the midst of a pandemic," said Nanshu Lu, an associate professor in the Department of Aerospace Engineering and Engineering Mechanics and the Wireless Networking and Communications Group (WNCG), who is leading the project.
The team was awarded $1.5 million over four years for the project, and the primary researchers include engineers, medical doctors, data scientists and more. They hope this interdisciplinary team will help knock down walls between specialties that keep medicine from advancing.
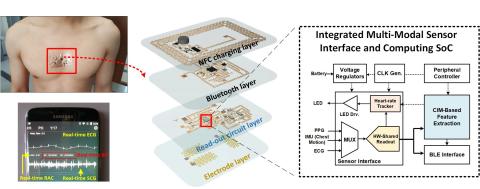
The researchers will make a hair-thin, skin-soft wireless wearable sensor, known as an electronic tattoo or “e-tattoo." This part of the project is led by Lu, who has been developing her e-tattoo technology for a decade at UT Austin.
An integrated system-on-chip will read out sensor signals and perform signal processing with ultra-low power consumption to ensure that patients can wear the device without interruption for at least a week on a single charge. Shaolan Li, an assistant professor in Georgia Institute of Technology's School of Electrical and Computer Engineering and a Ph.D. graduate from the Cockrell School, is handling this aspect of the project.
Li noted that he and his team at Georgia Tech have previously developed a few sensor interface integrated circuits that are designed to read biomedical signals like ECG or EEG with record-setting energy efficiency. He also added that he wants to leverage this knowledge to expand all of the capabilities of this new wearable device, aiming to profoundly advance the engagement of wearable electronics in clinical medicine. “Through this project, we really hope to showcase that the circuit technology innovation developed in our lab can truly address the most pressing problems that are facing humanity,” said Li.
A deep learning framework will be tailored to analyze all the data coming from the e-tattoo and predict how clinical condition progresses with evolution of the disease. Hongyu Miao, associate professor in the Department of Biostatistics and Data Science at The University of Texas Health Science Center at Houston, is leading the data science work and developing the deep learning tool.
And all this information will be managed through Sickbay, an FDA-approved virtual patient monitoring platform. Craig Rusin, associate professor at Baylor College of Medicine and head of the Predictive Analytics Lab at Texas Children’s Hospital, developed Sickbay. The program is used by hospitals across the country, including Texas Children’s, and he started the company Medical Informatics to commercialize it.
Parag Jain, a pediatric critical care physician at Texas Children’s Hospital and assistant professor of pediatrics at Baylor College of Medicine, will lead a clinical trial of the device. Using deep machine learning techniques, he will develop algorithms that can predict the progression of pneumonia using historical data. Once a prototype device is ready, likely in two to three years, the team will test it on 20 patients at Texas Children’s Hospital, aged 13 to 18 years, with progressive pneumonia.
The researchers targeted pneumonia for this project because it is a common illness, one that can be very dangerous, regardless of age or health status. As a side effect of not just COVID-19, but other respiratory viruses and bacteria, it is also quite prevalent. It also requires individualized care because each patient progresses differently.
The multi-faceted nature of the team illustrates the complexity of the problem they are trying to tackle. They are aiming to solve a challenging engineering problem as well as real-world issues with patient care.
Despite tremendous advances in medical technology, tools to continuously track and analyze all the data patients generate remain lacking. That often means that clinicians are only getting small snapshots of patients' condition, not the full picture.
This continuous monitoring and data analysis will allow medical personnel to use their time more wisely, to check in on patients at the most important moments. In critical cases of pneumonia, timing is everything, and the right treatment at the right time can make the difference between life and death.
"The pandemic really exposed gaps in care that patients with severe disease have to be treated using bulky, constrained, conventional monitors," Lu said. "We need sensors with ‘brains’ that can tell doctors when the time is right for that critical intervention, whether the patient is in a hospital bed just a few steps away or in their own home."
Additional Images